From Dr. Joseph Mercola
Since COVID-19 first entered the scene, exchange of ideas has basically been outlawed. By sharing my views and those from various experts throughout the pandemic on COVID treatments and the experimental COVID jabs, I became a main target of the White House, the political establishment and the global cabal.
Propaganda and pervasive censorship have been deployed to seize control over every part of your life, including your health, finances and food supply. The major media are key players and have been instrumental in creating and fueling fear.
I am republishing this article in its original form so that you can see how the progression unfolded.
Originally published: June 8, 2020
May 31, 2020, I posted an interview with three vitamin D experts in which we discuss the importance of vitamin D for preventing COVID-19 infection. A few days earlier, May 27, CNN published a report1 that could have deadly consequences if believed, claiming taking vitamin D supplements “can hurt a lot.”
The article was written by Sandee LaMotte — a medical producer and writer for CNN and executive producer of video at pharma-biased WebMD. Three other CNN reporters, Emma Reynolds, Shelby Lin Erdman and Rob Picheta, also contributed to the story.
The article quotes Robin May, director of the British Institute of Microbiology and Infection as saying:2 “To date, there is no evidence that very high vitamin D levels are protective against COVID-19 and consequently medical guidance is that people should not be supplementing their vitamin D levels beyond those which are currently recommended by published medical advice.”
CNN Cites Vitamin D Recommendations Known To Be Incorrect
LaMotte cites dosing recommendations from the Institute of Medicine’s National Academies’ Food and Nutrition Board — a nongovernmental organization — which advises a daily dose of just 600 IUs for anyone over the age of 4, and 800 IUs for those over 70. In the U.K., the daily dose is a meager 400 IUs a day.
Nowhere does the article mention that the IOM’s dosage recommendations are based on the levels thought to be adequate only for bone health.3 They do not take into account the amount of vitamin D you need to prevent influenza, heart- or liver- disease, respiratory infections, cancer, or any of the many other diseases that have a clearly documented link to vitamin D deficiency.
LaMotte also fails to mention that the IOMs recommendations are off by a factor of 10 due to a mathematical error, as reported by Science Daily4 in 2015. Two papers5,6 confronting this issue have been published in the journal Nutrients, both of which call for the IOM to correct its mistake, lest public health suffer.
So, if IOM were to simply go back and correct this egregious mistake, the “conventional medical advice” would be to take 6,000 IUs a day, or 8,000 IUs if you’re over 70. These dosages are quite close to the so-called “high-dose” recommendations suggested by many vitamin D researchers.
The statement that there is “no evidence that very high vitamin D levels are protective against COVID-19” is equally misleading, considering a number of reports from COVID-19 researchers now show that vitamin D appears to play a significant role in this infectious disease.
Similarly, researchers demonstrated that the age-specific case fatality rate of COVID-19 was highest in Italy, Spain and France — European countries with the highest incidence of severe vitamin D deficiency.7
In the video below, published May 11, 2020, on Medscape.com, Dr. JoAnn E. Manson, professor of medicine and chief of division of preventive medicine at Harvard Medical School, discusses the protective role of vitamin D against COVID-19.
Vitamin D Deficiency Increases Risk of Positive COVID-19 Test
A May 2020 paper8 published on the preprint server MedRxiv (which means it’s still awaiting peer-review) presents evidence that vitamin D deficiency increases the risk of testing positive for COVID-19 infection. As reported by News Medical Life Sciences:9
“The study by researchers at the University of Chicago looked at over 4,300 patients with COVID-19 of whom 499 had been tested for vitamin D levels in the previous year. Based on this, they were divided into likely deficient (25%), likely adequate (58%), and uncertain (16%).
Vitamin D deficiency was diagnosed by ‘the most recent 25-hydroxycholecalciferol <20ng/ml or 1,25-dihydroxycholecalciferol <18pg/ml within one year before COVID-19 testing.’
Multiple variables were analyzed in this study. The researchers found that people with vitamin D deficiency at the last testing, and who did not receive higher doses of vitamin D (keeping them deficient in all probability), are much more likely to be infected with the virus than those with probably sufficient levels. The corresponding rates of infection were 22% vs. 12%.”
Similarly, a May 6, 2020, report10 in the journal Nutrients pointed out that vitamin D concentrations are lower in patients with positive PCR (polymerase chain reaction) tests for SARS-CoV-2. As noted in this report, which retrospectively investigated the vitamin D levels obtained from a cohort of patients in Switzerland:11
“In this cohort, significantly lower 25(OH)D levels were found in PCR-positive for SARS-CoV-2 (median value 11.1 ng/mL) patients compared with negative patients (24.6 ng/mL); this was also confirmed by stratifying patients according to age >70 years. On the basis of this preliminary observation, vitamin D supplementation might be a useful measure to reduce the risk of infection.”
Low Vitamin D Boosts Risk of Serious COVID-19 Infection
According to an editorial review12,13 by Irish researchers, people with vitamin D deficiency appear to be far more prone to severe COVID-19 infections. According to the authors:14
“When mortality per million is plotted against latitude, it can be seen that all countries that lie below 35 degrees North have relatively low mortality. Thirty‐five degrees North also happens to be the latitude above which people do not receive sufficient sunlight to retain adequate vitamin D levels during winter. This suggests a possible role for vitamin D in determining outcomes from COVID‐19 …
There are considerable experimental data showing that vitamin D is important in regulating and suppressing the inflammatory cytokine response of respiratory epithelial cells and macrophages to various pathogens including respiratory viruses …
It is important to note that the hypothesis is not that vitamin D would protect against SARS‐CoV‐2 infection but that it could be very important in preventing the cytokine storm and subsequent acute respiratory distress syndrome that is commonly the cause of mortality …
The evidence supporting a protective effect of vitamin D against severe COVID‐19 disease is very suggestive, a substantial proportion of the population in the Northern Hemisphere will currently be vitamin D deficient, and supplements, for example, 1,000 international units (25 micrograms) per day are very safe.
It is time for governments to strengthen recommendations for vitamin D intake and supplementation, particularly when under lock‐down.”
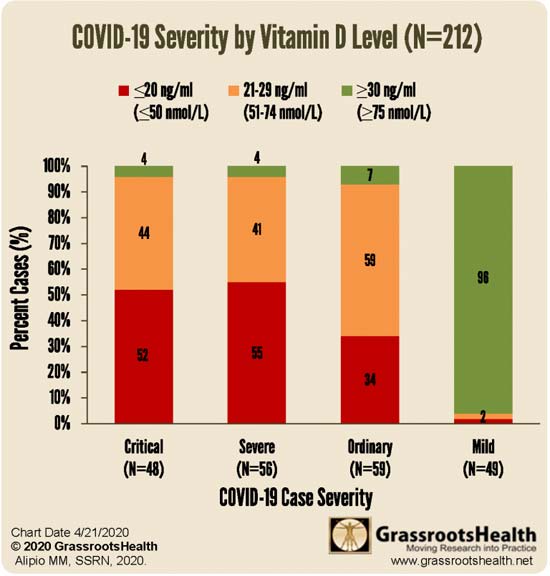
Similarly, Mark Alipio with GrassrootsHealth conducted a retrospective multicenter study15 involving 212 patients in Southeast Asia who had COVID-19. He too found a strong correlation between vitamin D levels and disease severity. Those with the mildest disease had the highest vitamin D levels, and vice versa.
Normal vitamin D levels were defined as greater than 30 ng/ml; insufficient levels were defined as 21 to 29 ng/ml; anything below 20 ng/mL was considered deficient. While Grassroots Health research has determined that 40 ng/mL is the lower edge of optimal, with 60 ng/mL to 80 ng/mL being ideal for health and disease prevention, the benefit of having a vitamin D level above 30 ng/mL was clear.
Low Vitamin D Levels Linked to Increased COVID-19 Mortality
The epidemiology of COVID-19 provides evidence that vitamin D might be helpful in reducing risk associated with COVID-19 deaths.16 A May 6, 2020, report17 published in Aging Clinical and Experimental Research (its prepublication featured in the Daily Mail May 118) found that countries with lower vitamin D levels also have higher mortality rates from COVID-19. According to the authors:19
“The Seneca study showed a mean serum vitamin D level of 26 nmol/L in Spain, 28 nmol/L in Italy and 45 nmol/L in the Nordic countries, in older people. In Switzerland, mean vitamin D level is 23 nmol/L in nursing homes and in Italy 76% of women over 70 years of age have been found to have circulating levels below 30 nmol/L.
These are the countries with high number of cases of COVID-19 and the aging people is the group with the highest risk for morbidity and mortality with SARS-CoV2.”
In the preprint version20 of this paper, the authors concluded: “We believe that we can advise vitamin D supplementation to protect against SARS-CoV2 infection.” In the final version,21 they toned down the recommendation to: “We hypothesize that vitamin D may play a protective role for COVID-19.”
Another study,22 which looked at data from 780 hospital patients in Indonesia, found those with a vitamin D level between 20 ng/mL and 30 ng/mL had a sevenfold higher risk of death than those with a level above 30 ng/mL, and having a level below 20 ng/mL was associated with a 12 times higher risk of death.
Vitamin D Is a Simple Strategy That Can Save Lives
In a May 18, 2020, letter23 to the Federal Chancellor of Germany, Angela Merkel, retired biochemist Bernd Glauner and Lorenz Borsche highlight these and other studies24 and ask whether a nationwide supply of vitamin D has been considered in Germany.
“Until a vaccine is available, vitamin D supplementation could be a preventive measure that should be discussed to reduce the lethality of covid-19. The available studies also suggest that vitamin D shock treatment may protect patients already infected and hospitalized with Covid-19 from lethal sepsis,” they write.
The following graph is included in the letter.
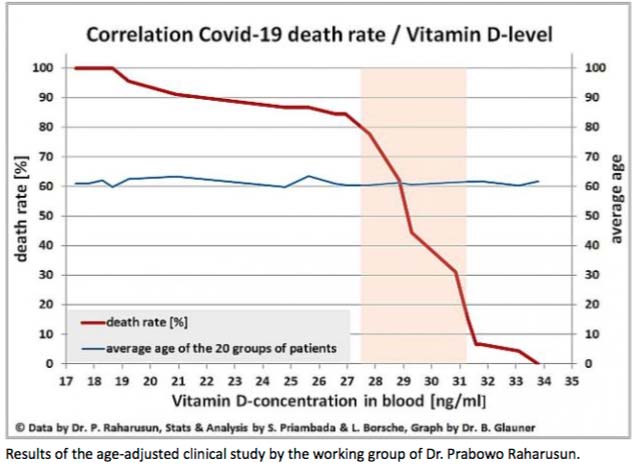
Glauner and Borsche continue:25
“… Scientific and clinical studies suggesting an alternative treatment option are apparently ignored. One of these promising approaches is the treatment with vitamin D. The available studies on Covid-19 patients suggest that a large proportion of deaths could possibly be prevented and severe courses could be reduced to milder ones …
This way would be easy and does not cause high costs. It would be sufficient to measure the vitamin D level in Covid-19 infected persons, hospital staff and risk patients and, if necessary, to raise it to healthy levels well above 35 ng/ml. In any case, no comparison to the enormous costs of the lockdown. This could possibly save us another lockdown and many more Covid-19 fatalities.”
No, Vitamin D Supplementation Is Not Dangerous
The CNN article is just another propaganda COVID-19 narrative of mainstream media. This egregious behavior is similar to the hydroxychloroquine paper published in The Lancet that the WHO has used to discredit and stop using hydroxychloroquine for COVID-19. Over 100 scientists question the ethics and standards of this incredibly shoddy study.26
Probably the most serious mistake in LaMotte’s CNN article are her claims that vitamin D supplementation “can hurt a lot.” She claims “too much vitamin D can lead to a toxic buildup of calcium in your blood, causing confusion, disorientation and problems with heart rhythm, as well as bone pain, kidney damage and painful kidney stones.”
She makes those claims without a) citing or referencing any supporting evidence, b) clarifying that the “toxic buildup of calcium” (hypercalcemia) is caused by insufficient vitamin K2 in relation to vitamin D, not vitamin D per se (a fact that is now well-established) and c) without specifying what “too much” actually might be.
A review27 of published trials have demonstrated there are no toxicity symptoms — including hypercalcemia — at dosages up to 10,000 IU of vitamin D3 per day, even when used long-term. A more recent paper found that Intakes of vitamin D up to 15,000 IU/day are safe.28
In my search for horror stories, I discovered a case paper29 published in 2011, which presented the cases of 10 adult patients diagnosed with hypercalcemia in relation to vitamin D supplementation.
Symptoms listed in this paper include vomiting, polyuria (excessive urination), polydipsia (excessive thirst), hypercalcemia (excessive calcium levels), encephalopathy (brain damage or disease causing memory loss, personality changes or seizures, for example) and kidney dysfunction.
It sounds scary, but when you consider that these patients were taking MILLIONS of units of vitamin D — specifically, 3,600,000 (3.6 million) IUs and 210,000,000 (210 million) IUs over the course of one to four months (median two months) — you start to see just how wrong it is to warn people off vitamin D supplements.
For example, the dosages these people were getting would be like taking 30,000 IUs of vitamin D per day for 120 days on the lowest end, or 7 million IUs a day for 30 days on the extreme upper end. No one is recommending you take these kinds of dosages, especially not for extended periods of time.
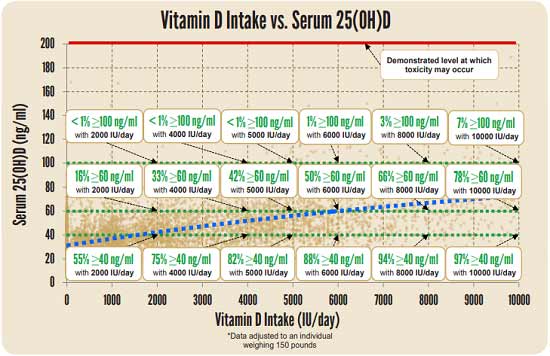
Many may need 10,000 IUs a day — which is safe — to get their level above 60 ng/mL. The maintenance dose, however, is typically lower. To determine your ideal dose, you need to get your blood tested, ideally twice a year. The level you’re looking for is between 60 ng/mL and 80 ng/mL. As of right now, there does not appear to be any significant benefit to levels higher than 80 ng/mL.
REALLY IMPORTANT: Optimize Your Vitamin D Level Before Fall!
Experts are already warning that SARS-CoV-2 may reemerge in the fall when temperatures and humidity levels drop, thereby increasing the virus’ transmissibility.
I am in the process of writing an even more comprehensive and detailed report on vitamin D in the prevention of COVID-19 and I hope to enlist ALL of you to participate as an army to go out and tell all your friends and family and get them on board to get their vitamin levels optimized.
Once you have done that, the next step is to encourage pastors of black churches to get their congregations on board. It will also be important to reach out to mangers of nursing homes and assisted living facilities as both of these populations have notoriously low vitamin D levels that put them at greater risk of COVID-19.
You now have a known “deadline” for optimizing your vitamin D level. Historically, December typically has highest flu activity in the U.S.,30 but it would probably be good to aim for October, or maybe even earlier depending on your location.
To improve your immune function and lower your risk of viral infections, you’ll want to raise your vitamin D to a level between 60 nanograms per milliliter (ng/mL) and 80 ng/mL by fall. In Europe, the measurements you’re looking for are 150 nanomoles per liter (nmol/L) and 200 nmol/L.
Again, optimizing your vitamin D is particularly important if you have darker skin, as darker skin places you at higher risk for vitamin D deficiency — and serious COVID-19 infection. What’s more, the elderly tend to lose the ability to synthesize vitamin D from sun exposure, and therefore tend to have suboptimal levels even if they spend plenty of time outdoors.
One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit, either alone or in combination with the omega-3 test. This is done in the convenience of your home.
You’ll learn your nutrient levels, how effective your health actions are, and you’ll be able to see thousands of other data sets that allow you to compare health outcomes important to you. Knowledge is empowerment, and that is particularly true during this pandemic. To make sure your immune system has a chance to work optimally, follow these three steps.
Step 1: Measure Your Vitamin D
First, find out what your base level is. This is done with a simple blood test. An easy and cost-effective way of doing this is to order GrassrootsHealth’s vitamin D testing kit.
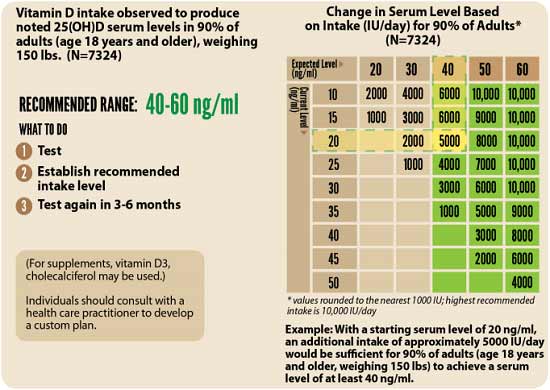
Once you know what your blood level is, you can assess the dose needed to maintain or improve your level. Again, the ideal level you’re looking for is above 40 ng/mL, and ideally between 60 ng/mL and 80 ng/mL (European measurement: 100 nmol/L or, ideally, 150 nmol/L to 200 nmol/L).
The easiest way to raise your level is by getting regular, safe sun exposure, but if you’re very dark-skinned, you may need to spend about 1.5 hours a day in the sun to have any noticeable effect.
Those with very light skin may only need 15 minutes a day, which is far easier to achieve. Still, they too will typically struggle to maintain ideal levels during the winter. So, depending on your situation, you may need to use an oral vitamin D3 supplement. The next question then becomes, how much do you need?
Step 2: Assess Your Individualized Vitamin D3 Dosage
The following chart can provide you with a basic starting point:
You can fine-tune your dosage further by taking into account your baseline vitamin D level. To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5.
How to Calculate Your Vitamin D From Sun Exposure
To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, consider using the DMinder app,31 created by Dr. Michael Holick, author of “The Vitamin D Solution: A Three-Step Strategy to Cure Our Most Common Health Problems.” The free app is available for iPhone and android in the Apple store and Google play respectively. As explained by imedicalapps.com:32
“The app attempts to calculate a patients’ vitamin D level based on demographics imputed when first opening the app and then updates the level based on either actual lab draws or data from the app. The app even uses the phone’s GPS and clock to determine the ‘best’ time of day for a patient to get the required sun exposure for vitamin D skin conversion.”
Step 3: Retest
Lastly, you’ll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you. Not only will optimizing your vitamin D be an important strategy for you and your family, but it would be really helpful to start thinking about your community as well.
If you can, speak to pastors in churches with large congregations of people of color and help them start a program getting people on vitamin D. Doing so could save far more lives than any vaccine program.
If you have a family member or know anyone who is in an assisted living facility you could meet with the director of the program and encourage them to get everyone tested or at least start them on vitamin D.

