The coronavirus pandemic exposed weaknesses in the U.S. health care system that existed before the public health crisis. What lessons can be learned from the COVID-19 stress-test to build American health care back better?
The National Academy of Medicine is publishing nine reports addressing health stakeholder segments impacted and re-shaped by COVID-19 — for public health, quality and safety, health care payers, clinicians, research, patients-families-communities, health product manufacturers, digital health, and care systems.
 The report on health care systems and providers was released this week: COVID-19 Impact Assessment: Lessons Learned and Compelling Needs was authored by experts on the front-line of health care delivery, medical education, and health policy.
The report on health care systems and providers was released this week: COVID-19 Impact Assessment: Lessons Learned and Compelling Needs was authored by experts on the front-line of health care delivery, medical education, and health policy.
The paper describes the landscape of the U.S. health system, including 637 health systems, two-thirds of which are not-for-profit and most operating in one state. Some 600,000 physicians provide care to people in the U.S. in nearly 4,000 hospitals that operate 600,000 inpatient beds.
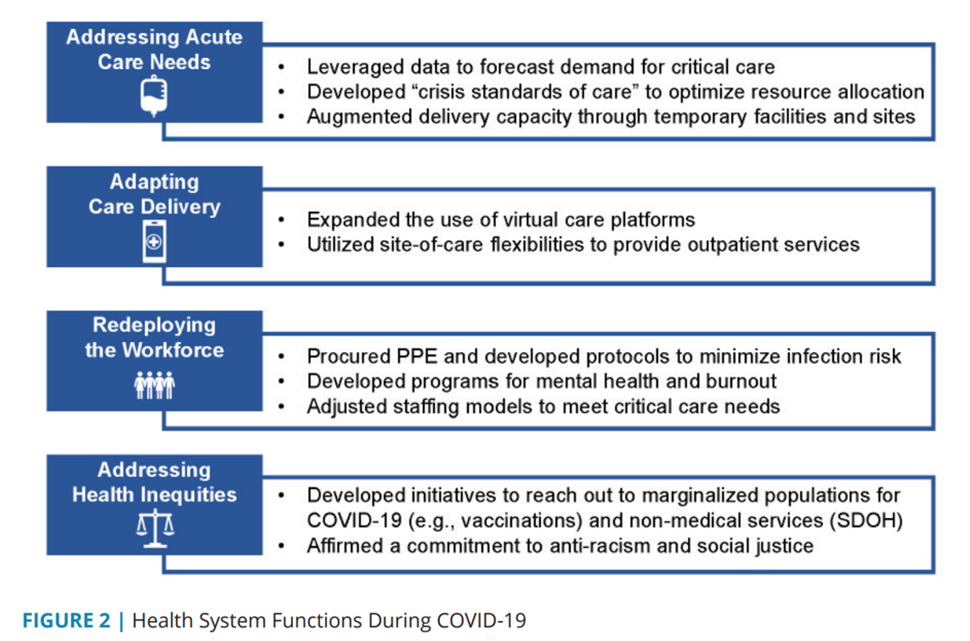
The first figure lists four key functions health systems experienced during COVID-19:
- Addressing acute care needs, re-allocating hospital resources toward critical and respiratory care, for example;
- Adapting care delivery, namely through launching or expanding existing virtual care/telehealth platforms;
- Re-deploying the workforce, moving staff to critical care from acute and ambulatory services and augmenting mental health human capital; and,
- Addressing health inequities. recognizing and re-committing energy and resources to social determinants of health and health justice.
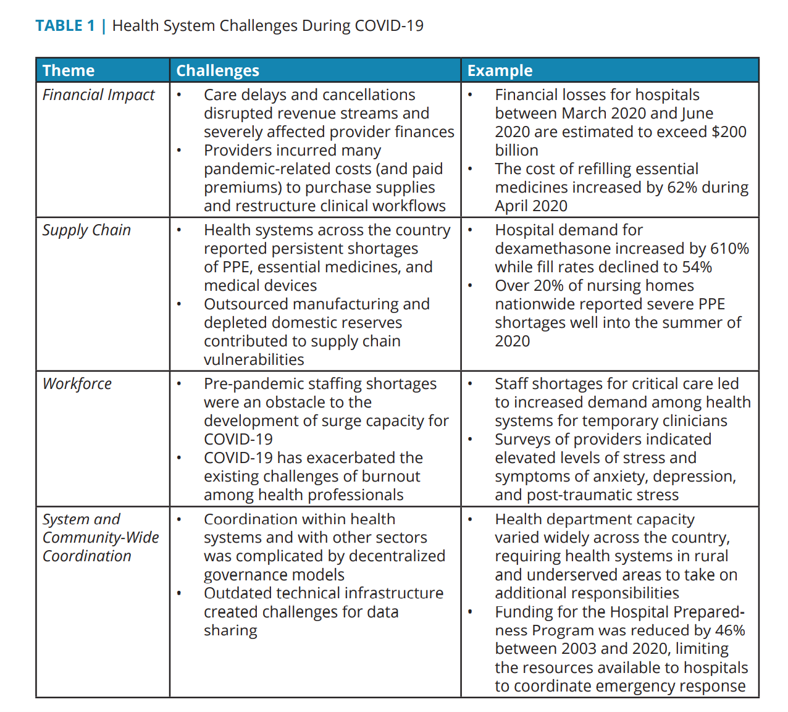 In taking on these four functions during the pandemic, hospitals and health systems faced many challenges in fast-adapting to the fast-moving public health crisis: financial, resulting in multi-billion dollar losses for U.S. hospitals; supply change shocks, especially for PPE, essential medicines, and medical devices (think: ventilators); workforce pressures, with staffing shortages and pandemic-related burnout among clinicians who had already entered 2020 with stress, anxiety and depression; and, system and community-wide coordination, which is a feature of U.S. health care — fragmentation between public health and acute care, inadequate health IT and information exchange, and lack of effective emergency response planning and coordination.
In taking on these four functions during the pandemic, hospitals and health systems faced many challenges in fast-adapting to the fast-moving public health crisis: financial, resulting in multi-billion dollar losses for U.S. hospitals; supply change shocks, especially for PPE, essential medicines, and medical devices (think: ventilators); workforce pressures, with staffing shortages and pandemic-related burnout among clinicians who had already entered 2020 with stress, anxiety and depression; and, system and community-wide coordination, which is a feature of U.S. health care — fragmentation between public health and acute care, inadequate health IT and information exchange, and lack of effective emergency response planning and coordination.
It became quite clear that health systems lacked preparedness for this emergency, begging the question about how to prep for future emergencies across the different kinds of gaps: financing, infrastructure, and coordination, and building effective and robust linkages between public health and health care systems, from ambulatory care through acute, post-acute, and long-term care, in rural areas and for safety-net providers.
 Health Populi’s Hot Points: The NAM report offers domain-specific recommendations that address the lessons learned in the pandemic, discussed above.
Health Populi’s Hot Points: The NAM report offers domain-specific recommendations that address the lessons learned in the pandemic, discussed above.
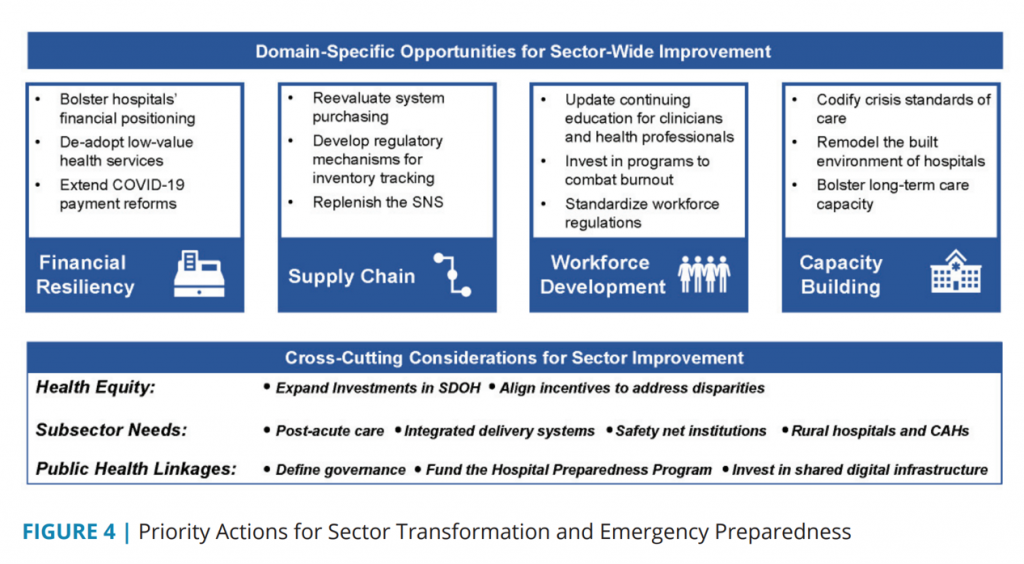
The four opportunity-areas focus on financial resiliency, shedding systems’ low-value health services and bolstering hospitals’ finances; supply chain, to ensure a full, robust Strategic National Stockpile for PPE and smarter purchasing processes; workforce development, investing in clinician well-being to mitigate burnout and advance continuing education; and, capacity building, re-imagining and re-building the built environment of hospitals and long-term care capacity.
Across these four domains, NAM points to “cross-cutting” considerations based on lessons learned in the pandemic:
- Health equity, aligning incentives to address disparities
- Subsector needs for post-acute care, rural health, and safety net providers, and
- Public health linkages, investing in shared digital infrastructure and defining governance and roles for accountability.
These three areas require investment and reallocation of resources in a health system that has long over-spent on acute care and under-invested in those upstream factors that bolster citizens’ well-being and social health: education (early and guaranteed), clean air and water, food security, housing security, and “good jobs” (think: income inequality and minimum working wage). As Dr. Michael Osterholm wrote in the May 5, 2005 issue of the New England Journal of Medicine, warning about “preparing for the next pandemic,”
“We need bold and timely leadership at the highest levels of the governments in the developed world; these governments must recognize the economic, security, and health threats posed by the next influenza pandemic and invest accordingly. The resources needed must be considered in the light of the eventual costs of failing to invest in such an effort. The loss of human life even in a mild pandemic will be devastating, and the cost of a world economy in shambles for several years can only be imagined.”
That was 2005.
At the 2021 South-by-Southwest Festival held in March 2021, I interviewed Dr. Michael Osterholm, Director of CIDRAP, the Center for Infectious Disease, Research and Policy housed at the University of Minnesota. Dr. O has been a prominent expert on COVID-19 and previous virus outbreaks, and was on President Biden’s COVID-19 Transition Advisory Board.
To hear Dr. Osterholm explain how the U.S. invests too little in public health infrastructure, especially in light of what we-know-we-know from our Year of COVID, here’s a link to our conversation….
