In the Fear of Going Out Era spawned by the COVID-19 pandemic, many patients were loath to go to the doctor’s office for medical care, and even less keen on entering a hospital clinic’s doors. This drove health consumers to virtual care platforms in the first months of the public health crisis — including lots of older people who had never used telemedicine or even a mobile health app.
In the August 2020 National Poll on Heathy Aging, the University of Michigan research team found a 26% increase in telehealth visits from 2019 to 2020, March to June 2020 year-over-year.
In May 2019, 14% of older patients’ health care providers offered telehealth visits, growing to 62% in June 2020 during the pandemic.
The survey was conducted online in June 2020 among 2,074 U.S. adults ages 50 to 80 years of age. AARP sponsored the poll.
This engaging video features commentary with researchers from U-M.
 The use of telehealth visits grew from 4% of older people having ever used virtual platforms by May 2019, to 30% of older patients using telehealth in June 2020.
The use of telehealth visits grew from 4% of older people having ever used virtual platforms by May 2019, to 30% of older patients using telehealth in June 2020.
Among these visits, 76% were with a primary care provider, 32% with a specialty care provider, and 18% with a mental health provider, the study found.
Most older patients who had a telehealth visit perceived the quality of an office visit was higher (56%) and offered better communication opportunity with the clinician (54%).
But a telehealth encounter was seen as more convenient than an office visit by 56% of older people.
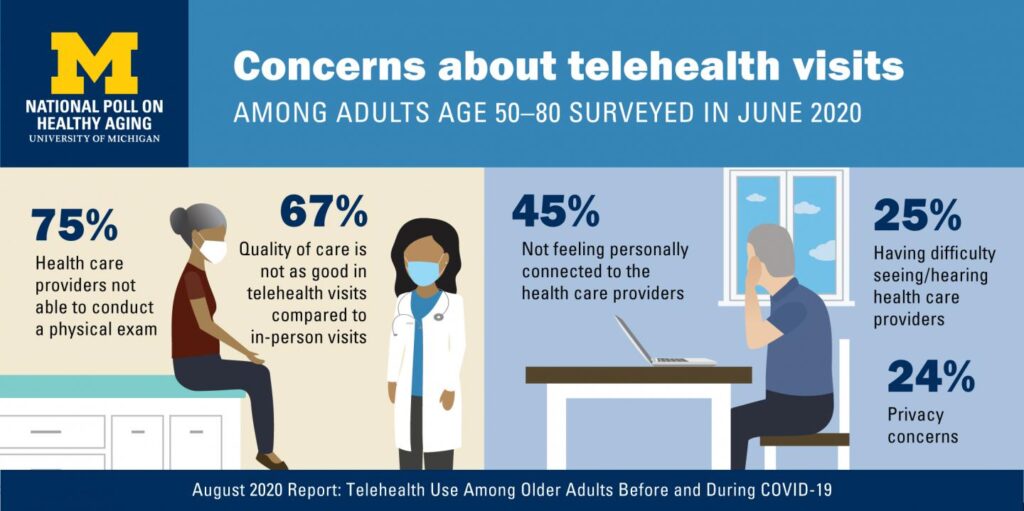
The study identified several key concerns about telehealth visits, shown in the graphic. These included:
- A clinician’s lack of ability to conduct a physical exam (75% of older people concerned about this)
- Quality of care not as good as in-person (among 67% of older people)
- 45% of older people did not feel personally connected to the virtual health care provider
- 25% had difficult seeing or hearing the clinicians
- 24% had privacy concerns.
On the upside, most older people were comfortable with using video conferencing technologies, a proportion rising from 53% in May 2019 to 64% in June 2020. And, by June 2020, fewer older people reported having never used FaceTime, Google Hangout, Skype and other video conferencing technologies, dropping from 28% never using the tech’s in May 2019 to 17% by June 2020.
Furthermore, building the positive case among older peoples’ demand for telehealth in the future, two-thirds said they would be interested in a telehealth visit for a one-time follow-up visit after a medical procedure or surgery, and those who had had a past telehealth visit were more likely than people who hadn’t to be interested in future virtual visits for primary care and specialty care. Four in ten older people who had experienced telehealth also said they would be interested in telehealth for mental health care in the future.
Health Populi’s Hot Points: The COVID-19 pandemic will persist well into 2021 based on current projections, and the health care system will continue to adapt to both clinical workflows and the public health guidance for physical distancing and hygiene. The latter have impacts on the former in terms of managing patient-density in physical spaces, scheduling time in procedure rooms, and dealing with high-risk patients who must mindfully risk-manage their exposure to the virus.
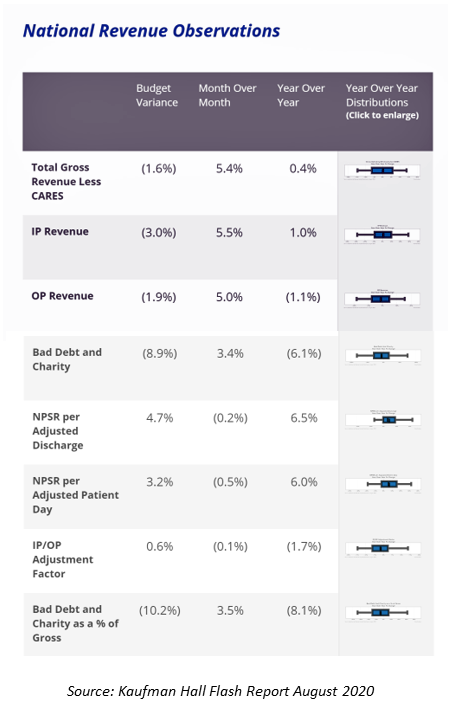 The latest Kaufman Hall Flash Report, published August 2020 with July data, demonstrate continued fiscal challenges for the hospital sector that will continue into the autumn 2020. Depending on the trajectory of the U.S. flu season, hospitals may encounter further financial challenges due to the convergence of the coronavirus with the flu virus. Kaufman Hall notes that, “While the year-to-date increases in actual expenses are minimal, they show that expenses are increasing even as hospitals are seeing fewer patients. Once adjusted for volumes, the higher expenses are more evident as hospitals struggle to hold down per-patient costs.” The report’s revenue data is shown here in a table from Kaufman Hall’s analysis of the July 2020 data.
The latest Kaufman Hall Flash Report, published August 2020 with July data, demonstrate continued fiscal challenges for the hospital sector that will continue into the autumn 2020. Depending on the trajectory of the U.S. flu season, hospitals may encounter further financial challenges due to the convergence of the coronavirus with the flu virus. Kaufman Hall notes that, “While the year-to-date increases in actual expenses are minimal, they show that expenses are increasing even as hospitals are seeing fewer patients. Once adjusted for volumes, the higher expenses are more evident as hospitals struggle to hold down per-patient costs.” The report’s revenue data is shown here in a table from Kaufman Hall’s analysis of the July 2020 data.
Doctors’ practices, too, will continue to pivot to virtual care, discussed yesterday in Health Populi in the context of the 2020 Physicians Foundation survey of doctors in the COVID-19 era.
A growing proportion of older patients are engaging in virtual health care visits, and once experienced, patients are generally open to more telehealth in their personal mix of medical services in certain situations — to follow up procedures, for repeat primary care and chronic care follow-up, and increasingly, for telemental health.
Virtual care will be a lifeline for many older people who cannot leave home or do not want to do so. In my new book on Health Citizenship, to be published in September 2020, I document the growing ethos among many health consumers I coin as the “fear of going out” — the opposite life-flow to some peoples’ “fear of missing out,” or FOMO. FOGO has creeped into many patients’ mindsets for self-preservation and risk-management of the coronavirus — in particular, among people with pre-existing conditions that compromise immunity or increase risk for coronavirus complications, and among people who live with older people at greater risk for COVID-19 illness.
Because telehealth becomes a lifeline for some people, it is part of the social determinants of health portfolio which bolster, or diminish, peoples’ health. Virtual care, especially in a pandemic, is important for older people to have as a go-to for medical care when clinically appropriate.
The University of Michigan identified several concerns older patients felt in the telehealth experience: among them, perceived quality, a feeling of personal connection, seeing and hearing in communications, and embedded privacy-by-design in the technology platform that would be visible to patients.
We must laud and appreciate clinicians’ fast-adoption of telehealth from a very low use rate in 2019 to fast-growth in 2020. Now that virtual care programs have been stood up, fine-tuning and re-designing must commence to improve these systems for patients beyond the pandemic crisis. In addition to user-centered design principles for the technology platforms and processes, clinicians also need to consider “webside manner” in the real-time exam setting. Communicating via video conference technology is not the same as in-person encounters, and older patients have identified this deficiency in the virtual visit in the U-M study.
Doctors aren’t alone in stretching these new muscles in learning to communicate and show empathy via Skype, Zoom, Microsoft Meetings, and telemedicine platforms. Those of us who teach, do business via tele-work, coach us in yoga from a distance, conduct religious services, and everyone making the pivot to working-from-home, learning-from-home, and praying-via-video, are all adapting…together, in this next-normal for health and daily living.
