Have you ever wondered what pain is like? The uncomfortable feeling somehow can cause pain for any degree. A sensation of pain, discomfort, tingling, burning, or damage within the spinal cord and brain indicates that something is wrong with your body. That’s when your nerves send to you a warning stimuli message. It starts with nerve endings and spinal cord and passes the message to the brain and body part. Below in our skin are thousands of cells called nociceptors (pain receptors)[1]. That detects light, cold, heat, pressure, touch and pain. Most of the receptor cells detect pain. Some of them feel cold.
Pain management is a surprisingly challenging, complex balancing act. Overtreating pain, for example, runs the risk of addicting patients to pain medication. Undertreating pain, on the other hand, may lead to long-term chronic pain and other complications. Today, doctors generally gauge pain levels according to their patients’ own reports of how they’re feeling. But what about patients who can’t communicate how they’re feeling effectively — or at all — such as children, elderly patients with dementia, or those undergoing surgery? Here in this article, let’s find out about pain receptors by discriminating the different types of pain, and see how pain receptors react to it.
About Pain receptors (Nociceptor)
“We do not have the pain receptors,” says pain specialist neuroscientist Lorimer Moseley. The pain comes not from the sense region, but the meaning, expectations, previous exposure, cultural norms / Social / beliefs of the hazard assessment of the brain. Pain, as defined by the International Association for the Study of Pain[2], is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage.” It is claimed that pain is a localized emotion.
What are pain receptors?
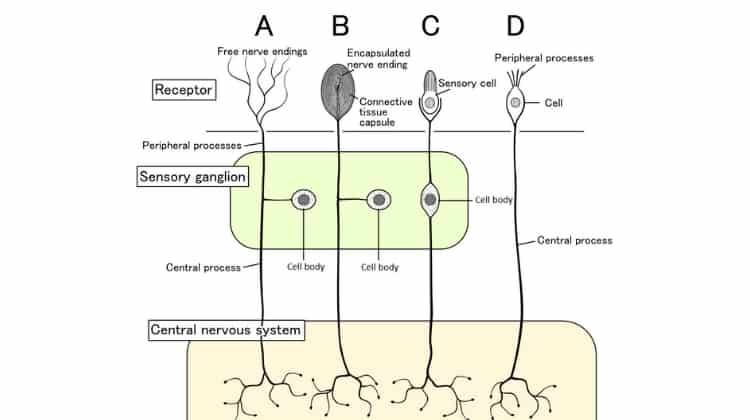
Pain receptors – are often called Nociceptors[3]. They are the free nerve endings located throughout the body, including the skin, muscles, joints, bones and internal organs. They play an important role on how you react to pain. The objective of the nociceptor is to respond to the body damage by sending signals to the spinal cord.
Note, these transmit pain signals are complex, bringing information on the location and intensity of painful stimuli. In this way, the brain can fully process the pain and subsequent communication eventually send other signals to block pain.
Where are pain receptors located?
Humans have a broad nervous system, which is the basis of sensation and many tasks, muscle movement and coordination. Pain is a sensation that normally happens in association with any type of pain. The trauma typically occurs as a result of nerve signals and relays chemicals released[4] stimuli, starting with specific pain receptors. These exist in almost all nerve endings although tend to be more prolific in skin, muscle and joints; they are also common in connective tissues and internal organs.
How do we sense pain?
The scientists gradually uncover the process in the body that causes the unpleasant sensation of pain. You stab your finger on something sharp. This causes tissue injury, which can capture the microscopic pain (nociceptors) in your skin. Every pain receptors form one end of the nerve cell (neurons). It connects to the other end in the spinal cord by long nerve fibre or axons. When the pain receptor is active, it sends an electric signal to nerve fibers.
Nerve fiber[5] is packed with many others to form a peripheral nerve. The electrical signal passes to the neuron in the peripheral nervous system to reach the spinal cord in the neck.
In an area of the spinal cord known as the dorsal root ganglia the electrical signals are transmitted from one neuron to another via the connections (synapses) by means of chemical messengers (neurotransmitters)[6]. The signals then goes to the spinal cord to the brain.
In the next step, that signal goes to the thalamus. This is a sorting station that relays signals to different parts of the brain. A signal transmit to the somatosensory cortex (responsible for the physical sensations), the frontal cortex (responsible for thought), and the limbic system (associated with emotion).
Which of the receptor types might function as a nociceptor?
Not all nociceptors[7] respond in the same manner and with the same intensity to noxious stimuli. There are several categories, depending on their responses to mechanical, thermal or chemical stimulation. Curiously, one distinguishing characteristic is that prolonged stimulation can sensitize nociceptors, then begins to respond to different sensations.
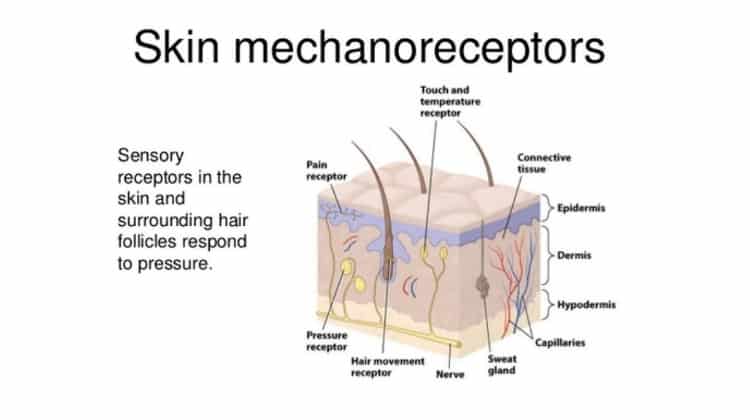
Nociceptors of the skin or cutaneous ( sensory receptors )
Transmission of nociceptive signals triggers when the network detects various types of noxious stimuli injuries, such as compression or intense heat. We can tell apart this type of nociceptors by four categories according to their function:
- Mechanical Nociceptors (mechanoreceptors): Nociceptors mechanically activate from intense tactile sensation, such as puncture, pressure, or deformation; therefore, they respond to cuts and bruises
- Thermal Nociceptors (thermoreceptors): Thermal stimuli activated when we contact a surface or an element of a very high temperature. We often experience this painful sensation without even knowing what happened or what touched.
- Chemicals (chemoreceptors): Chemical nociceptors respond to different chemical stimuli compounds that release in the face of an infection, inflammation, or disease. These are substances such as bradykinin, and histamine which reach the blood when we suffer an injury, when the wound is infectious.
- Polymodal: polymodal nociceptors respond to different stimulation types: thermal, mechanical, and chemical. Lead pain signals through, significantly slower than the fibers C fibers. We can find this type of nociceptors in the dental pulp, among other body parts.
Nociceptors of the joints
Joints and ligaments have high threshold mechanoreceptors, polymodal nociceptors and silent nociceptors. Some nerve fibers containing these receptors have neuropeptides such as substance P or peptide associated with the calcitonin gene.
These released substances seems to be a development of inflammatory arthritis. In muscles and joints are also nociceptors-δ type A and C. The first are active when sustained muscle contractions. While responding C to heat, pressure and ischemia.
Visceral nociceptors
The organs in our body have receptors that detect temperature, mechanical stress and chemicals containing silent nociceptors. visceral nociceptors that spread out from each other a few millimeters apart. Although, in some organs, there may be a few centimeters between each nociceptor.
All data captured by harmful viscera and skin goes to the central nervous system through different routes.The vast majority of visceral organ nociceptors have myelinated fibers. Two classes can be distinguished: the high activation threshold fibers which are active, and those non-specific. This can turned against both innocuous and noxious stimuli.
Silent nociceptors
This is the kind of nociceptors staying in the skin and in the tissue. These nociceptors got these names because they are at rest, ie, they usually do not respond to noxious stimuli mechanically.
However, they can “wake up” and begin to respond to mechanical stimulation after injury or during inflammation. This may be due to the continual stimulation of the injured tissue lowered threshold for this type of nociceptors, causing it to begin to respond.
Does The Brain Have Pain Receptors?
There is no pain receptor in the brain itself. Brain cannot really feel pain, as it lacks sensory receptors for pain (nociceptors). However, what you feel when you have a headache is not the brain can feel pain. There are many other areas on the head and neck that have nociceptors that perceive pain, and literally cause pain.
In fact, the brain contains layers of coatings, blood vessels, scalp and some muscles. All these other structures have pain receptors. The brain coverings are called meninges and consist of the arachnoid, pia and dura. The dura in particular has many receptors of pain and can be responsible for headaches.
In particular, many types of pain in the brain such as headaches and migraine have a neurovascular background, and responsible pain receivers are associated with blood vessels.
Even though the brain does not have nociceptors, a headache can still indicate a problem with the brain. Headaches that prolong and do not respond to drugs, or become sudden and extraordinarily serious, can be signs of a serious problem with the brain such as a tumor, bleeding, or infection. Although these problems cause pain, it is activating the nociceptors in the brain itself because the brain swells and presses to other structures in the head.
Neural pathways for pain
Active receptors respond to a kind of stimulation, both internal or external. Prick a finger with a pin is an example of external stimulation, while something like a twisted bowel or intestine is blocked internally. The receivers at the ends of the closest nerve stimulation which this occurs are generally responsible for cataloging it. The nerve signal sends it to the main nervous system and, ultimately, to the brain regions.
When tissues or other body parts are damaged, these will emit chemical substances known as “second order messengers“[8]. Second order important messengers include bradykinin, prostaglandins, histamine, serotonin, leukotrienes, and potassium. The nerve endings detect their presence in the environment that normally activate their pain signal centers.
The science behind this can be a bit tricky, but often makes more sense when taken as “nerve by nerve”. The fibers of the peripheral nerve containing these types of receptors are afferent nerves. This means that the brain and spinal cord can receive the nerve cell impulses signal. There are two main types of primary afferent nociceptors[9] in the tissues: A-delta and C-fiber sensory.
A-delta Fiber
A-delta fibers[10] are myelinated nerves, which means that they are covered by a protective shield slippery; as a result of these nerves transmit pain signal impulses generally very fast pain receptors on A-delta fibers activated in response to a sharp, localized pain that requires immediate reaction. Kind of painful stimulus sometimes relates to as “somatic pain,” and usually involves damage to the skin or muscle.
C-fiber
In contrast, C-fiber[11] sensory pain receptors that are activated in response to a dull, aching, or local bad pain stimuli. The unmyelinated pain fibers, and as a result of nerve impulses goes more slowly. C-fiber sensory nerves respond to the so-called “visceral pain,” which usually occurs with a damage to internal organs.
After the second messenger, stimulus goes along afferent nerves to go through the dorsal horn of the spinal cord. This is called a “relay station” [12] for the pain pathway and where a painful stimulus is transmitted to the various parts of the brain. Some pain impulses goes directly to the thalamus and brain stem for rapid response, while others runs to the brain’s frontal cortex for further processing. It is in the frontal cortex that the conscious realization of lasting pain.
Detecting Pain Levels Via Brain Signals
Researchers from MIT and elsewhere have developed a system that measures a patient’s pain level by analyzing brain activity from a portable neuroimaging device. The system could help doctors diagnose and treat pain in unconscious and noncommunicative patients, which could reduce the risk of chronic pain that can occur after surgery.
In a paper presented at the International Conference on Affective Computing and Intelligent Interaction, the researchers describe a method to quantify pain in patients. To do so, they leverage an emerging neuroimaging technique called functional near infrared spectroscopy (fNIRS), in which sensors placed around the head measure oxygenated hemoglobin concentrations that indicate neuron activity.
For their work, the researchers use only a few fNIRS sensors on a patient’s forehead to measure activity in the prefrontal cortex, which plays a major role in pain processing. Using the measured brain signals, the researchers developed personalized machine-learning models to detect patterns of oxygenated hemoglobin levels associated with pain responses. When the sensors are in place, the models can detect whether a patient is experiencing pain with around 87% accuracy.
Traditionally, surgery patients receive anesthesia and medication based on their age, weight, previous diseases, and other factors. If they don’t move and their heart rate remains stable, they’re still fine. But the brain may still be processing pain signals while they’re unconscious, which can lead to increased postoperative pain and long-term chronic pain. The researchers’ system could provide surgeons with real-time information about an unconscious patient’s pain levels, so they can adjust anesthesia and medication dosages accordingly to stop those pain signals.
Focusing on the forehead
In their work, the researchers adapted the fNIRS system and developed new machine-learning techniques to make the system more accurate and practical for clinical use.
When a patient is hurt, regions of the brain associated with pain will see a sharp rise in oxygenated hemoglobin and decreases in deoxygenated hemoglobin, and these changes can be detected through fNIRS monitoring. But traditional fNIRS systems place sensors all around the patient’s head. This can take a long time to set up, and it can be difficult for patients who must lie down. It also isn’t really feasible for patients undergoing surgery.
Therefore, the researchers adapted the fNIRS system to specifically measure signals only from the prefrontal cortex. While pain processing involves outputs of information from multiple regions of the brain, studies have shown the prefrontal cortex integrates all that information. This means they need to place sensors only over the forehead.
Personalized pain modeling
In the test, each participant wore the researchers’ fNIRS device and randomly experienced to an innocuous sensation and then about a dozen shocks to their thumb at two different pain intensities, measured on a scale of 1-10: a low level (about a 3/10) or high level (about 7/10). The result is, the participants self-reported the low level as being only strongly aware of the shock without pain, and the high level as the maximum pain they could tolerate.
In training, the model extracted dozens of features from the signals related to how much oxygenated and deoxygenated hemoglobin present, as well as how quickly the oxygenated hemoglobin levels rose. Those two metrics — quantity and speed — give a clearer picture of a patient’s experience of pain at the different intensities.
Importantly, the model also automatically generates “personalized” submodels that extract high-resolution features from individual patient subpopulations. Traditionally, in machine learning, one model learns classifications — “pain” or “no pain” — based on average responses of the entire patient population. But that generalized approach can reduce accuracy, especially with diverse patient populations.
The researchers’ model instead trains on the entire population but simultaneously identifies shared characteristics among subpopulations within the larger dataset. For example, pain responses to the two intensities may differ between young and old patients, or depending on gender. This generates learned sub-models that break off and learn, in parallel, patterns of their patient subpopulations. At the same time, however, they’re all still sharing information and learning patterns spreading across the entire population. In short, they’re simultaneously leveraging fine-grained personalized information and population-level information to train better.
Frequently Asked Questions
Yes. Health care providers classify pain by its duration (how long it lasts), its quality (how it feels) or by location (where in the body and where it originated, it is felt). Acute pain (ie, pain of recent onset length or short) usually has a clear source, it starts suddenly and disappears quickly. Chronic pain can last for months or years. You can come and go or remain constant. In addition, you may experience sleep disturbances, decreased appetite and lead to depression.
Other organs, such as the intestine and muscles, have less pain receptors. . It is interesting to note that the brain itself does not have pain receptors at all, and therefore not sensitive to pain. The pain receptors are free nerve endings.
In addition to the type of nociceptive that responds to stimuli, nociceptors are also classified by how fast they transmit pain signals. This transmission rate is determined by the type of nerve fibers (called an axon) is one nociceptor.
Both somatic pain and visceral pain [13] are detected by the nociceptors, the sensory nerves that detect acute pain due to tissue injury, and chronic pain due to swelling or inflammation.
